Abstract
Cancer patients sometimes choose intravenous nutrient treatments as a component of, or as the entire, treatment plan for their cancer. In 2018, 111 of a naturopathic cancer clinic’s patients received intravenous nutrient therapy, and answered a questionnaire regarding their frequency of exercise, subjective wellbeing, and feeling of strength. Patients’ responses were compared regarding their stage of cancer, and history of chemotherapy, radiation and surgery. Surgery prior to naturopathic treatments was found to have no significant correlation with frequency of exercise during naturopathic treatment. But prior chemotherapy and prior radiation both correlated with less frequent exercise during naturopathic treatment.
Background
Nature Works Best is a naturopathic cancer clinic in Tempe, AZ. None of the conventional cancer therapies are used at our clinic. However, each patient is encouraged to make their own decisions regarding whether and to what extent to use any of the conventional cancer therapies outside of our clinic. No outside therapy is known to be incompatible with any of our treatments. Most patients at our clinic have chosen not to have chemotherapy, and most have chosen not to have radiation. Far fewer choose to have either of those treatments simultaneously with the naturopathic treatments. Roughly one half have chosen to have surgery. Table 1 below shows the numbers and percentages of patients who choose each of the major conventional cancer treatments.
Each year since 2009 our clinic has reported confidentially the results that we have learned for all of our patients.[1]
From 2009 until 2014, we published follow-up results for all clinic patients who stayed at least 2 weeks in our care, including events of remission or death, when applicable. As the number of previous patients accumulated over those years, it became more difficult and labor intensive to contact each person, or to try to compare patient results when many variables were significant.
For example, it is not optimal to compare the results of those who had current imaging with those who have chosen to postpone imaging. Generally, it has been difficult to compare results of those who maintain an ongoing interest in their prior cancer diagnosis with those who prefer to distance themselves from that time. Specifically, some choose to maintain updated labs or imaging, but there are even more former patients who would prefer not to be reminded of that past experience and who tend to defer labs and imaging.
Therefore, in 2015 we began focused questionnaires each year of current patients regarding their current circumstances, while receiving treatments at our clinic.
The topic of this paper is the information gathered from patients who completed our 2018 questionnaire, which focused on questions of exercise frequency and self-reported wellbeing during the time that they were undergoing treatment at our clinic for cancer.
Methods
In 2018, we asked current clinic patients the following questions:
How many times per week do you exercise?
Do you feel . . .? Very strong, strong, medium, weak or very weak
How are you? Excellent, very good, good, okay or bad
What was your stage of cancer (at its worst)?
Have you had . . . Previous chemotherapy? Previous radiation? Previous surgery?
Results and analysis
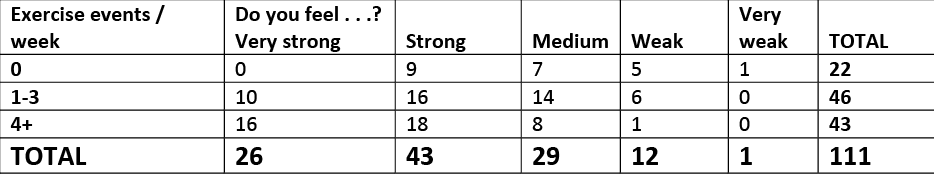
The following tables display most possible permutations of these question combinations.
Table 1 breaks down, by stage, the previous treatments that our 2018 patients had prior to arriving to our clinic. There is some overlap among treatments. That is, some patients had more than one of the following conventional treatments, which is why, for example, the 45 Stage 4 patients have 19 who had previous chemotherapy, 21 who had previous radiation, and 22 who had previous surgery. Those numbers add up to more than 45, because some people had multiple conventional treatments.
Table 1
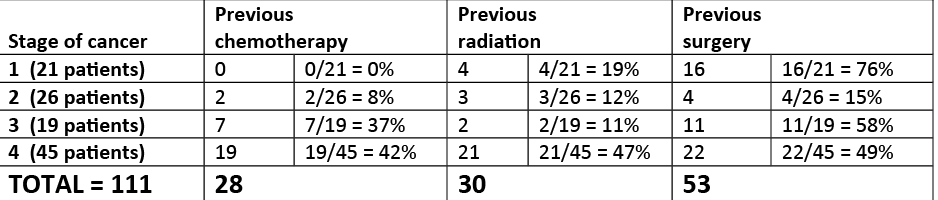
40 total patients had chosen to have none of the conventional treatments (12 of Stage 1, 10 of Stage 2, 5 of Stage 3, and 13 of Stage 4).
Table 2 compares patients who exercised 0, or 1 to 3, or 4+ times per week, first regarding the average stage of cancer. Then those same groups are compared for percentage of those who previously had chemotherapy treatments, radiation treatments or surgery for their cancer.
Table 2
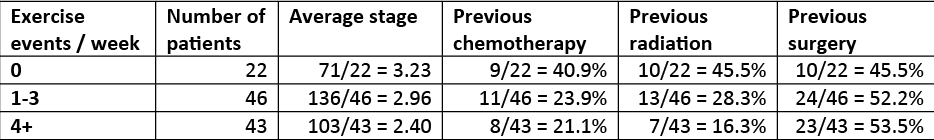
We have assumed that frequency of exercise to some extent measures wellbeing and overall strength. This correlation may be confounded by the degree of motivation to get well, prior thoughts and beliefs about exercise benefits, prior habits of exercise before cancer diagnosis, current availability of one’s favorite forms of exercise, and encouragement or discouragement of exercise by others.
Regarding exercise and stage of cancer, it is not surprising that those in the earlier stages of cancer were able to exercise more. That is, we see that for the more exercise activities per week, we see a somewhat lower stage of cancer.
However, the difference in average cancer stage between maximally exercising (4+ times) and minimally exercising (0 times), was less than one numerical stage of cancer. (3.23 – 2.40 < 1.) This implied that exercise for cancer patients may have some component of choice and motivation, as opposed to, or in addition to, simply wellbeing and the ability to exercise. Because cancer is generally staged only from one to four, it is not especially surprising that this difference is less than one.
Previous chemotherapy seemed to play an ongoing and overall deleterious role in the patient’s ability to exercise. Those who did not exercise at all were much more likely (almost 2x as likely) to have previous chemotherapy than those who exercised 4 times per week or more.
This difference was even more pronounced with previous radiation, where we see an even wider spread of previous radiation among those exercising 0, 1 to 3, and 4+ times per week. That is, we see that those who did not exercise at all were much more likely (almost 3 times as likely) to have had previous radiation than those who exercised 4 times per week or more. This implies an even more weakening long-term effect of radiation than of chemotherapy.
However, very interestingly, previous surgery seemed to have the opposite effect: Patients who exercised more were actually somewhat more likely to have had previous surgery for their cancer.
The differences in likelihood of previous surgery among the different exercise groups is too slight to be significant in itself. However, what interests us is that we do not see with previous surgery the large spread of – or even any at all – negative correlation with exercise activity that we see with previous chemotherapy and with previous radiation.
At this clinic we have long observed that surgery seemed to be a useful, and mostly successful, adjunct to the treatments that we give patients. Surgical resection of tumors combined with the intravenous nutrient treatments at our clinic have generally shortened patients’ treatment time with us, often by about half, that is generally 3 months of treatment as opposed to 6 months or longer. Also, the IV nutrient treatments following surgery have enabled fast recovery from surgery. This is most likely due to the fact that Vitamin C, which is one of the main nutrients used, is necessary for collagen formation and tissue repair, enhanced by the synergy of the multiple nutrients used in their treatments.
On the other hand, current and former chemotherapy patients have been long observed at our clinic to have a harder time achieving remission than those who never had chemotherapy. Chemotherapy is known to impart resilience to cancer[2], and to increase the likelihood of metastases.[3] Therefore, it is not really surprising that patients with previous surgery were better able to exercise, but that those who used the other conventional treatments exercised less.
However, there is likely another factor that may be more relevant: Chemotherapy and / or radiation are offered to almost all cancer patients. However, surgeons have generally been more selective in their patients, offering surgery only to those whose tumor burden is likely to be fully resected. Surgery is not always offered to Stage 4 cancer patients, or those with tumors in difficult, precarious, or highly vascularized areas. Many times surgery is only offered after some rounds of chemotherapy, which regimen patients do not always survive. That may help to explain the difference that appears in the last column in the table, from the previous two columns (surgery vs. chemotherapy or radiation).
We asked questions regarding wellbeing and strength, Tables 3 and 4.
Table 3
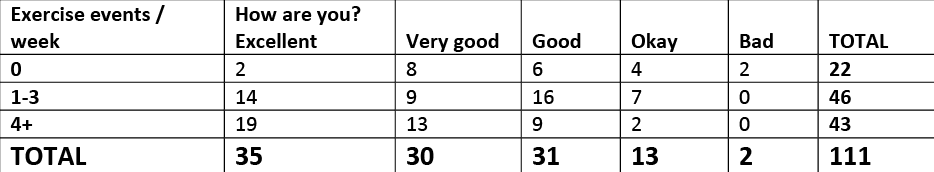
Table 4
It is not surprising that the people who feel well and strong choose to exercise more than those who feel poorly and weak, as reflected in the above two tables. This suggests that exercise is done somewhat more by ability than by choice, motivation or relative convenience.
Table 5 compares subjectively reported wellbeing among the various stages of cancer.
Table 5
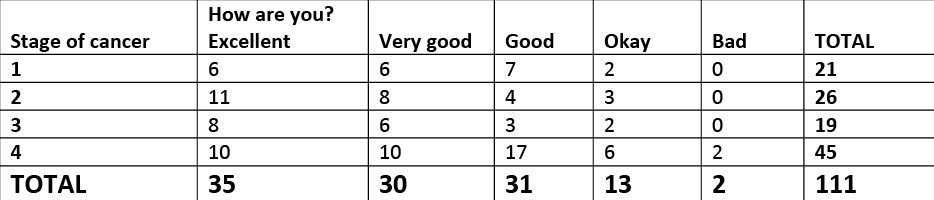
As expected, early stage cancer patients mostly felt “excellent,” “very good” or “good.” We also note that many more Stage 4 cancer patients felt “excellent,” “very good” or “good” than “okay” or “bad.” (37 vs 8). This is likely due to the lack of side effects and high tolerability of our treatments, as well as their cancer-disrupting and nourishing effects on the individual.
Table 6 compares feelings of strength among patients in the various stages of cancer diagnosis.
Table 6
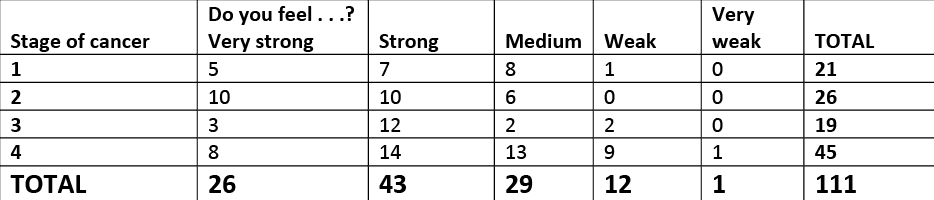
We also noted that, although Stage 4 cancer patients are by far the largest group by stage, of clinic patients, the majority felt either “very strong,” “strong” or “medium” versus “weak” or “very weak. (35 vs 10).
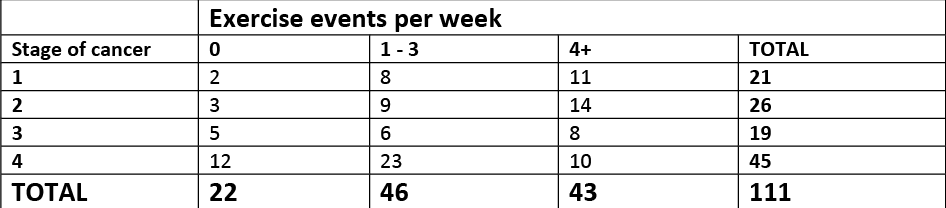
Table 7 compares the frequency of exercise among those with various stages of cancer. We see that even the majority of the stage 4 patients exercised at least once per week (33 vs 12).
Table 7
Conclusion
Cancer patients, stages 1 through 4, treated with
intravenous nutrients, were mostly able to exercise, and reported generally
positive wellbeing and strength. Surgery
has been a useful and successful adjunct to those treatments. Chemotherapy and radiation did not show to be
as helpful, when considered by measures of wellbeing and frequency of exercise.
[1] Huber C. Defeating cancer requires more than one treatment method. 2017 update. /wp-content/uploads/2018/01/2017-Cancer-treatment-paper.2017.12.30.pdf
[2] Luqmani Y. Mechanisms of drug resistance in cancer chemotherapy. Med Princ Pract 2005; 14 Suppl 1:35-48. https://www.ncbi.nlm.nih.gov/pubmed/16103712
[3] Karagiannis G, Pastoriza J, et al. Neoadjuvant chemotherapy induces breast cancer metastasis through a TMEM-mediated mechanism. Science Translational Medicine, Jul 2017. 9 (397). http://stm.sciencemag.org/content/9/397/eaan0026.short